The Brief
Hitch was commissioned by The English HIV and Sexual Health Commissioners Group (EHSHCG) to deliver in-depth research to build intelligence around the use of Pre-exposure prophylaxis (PrEP). PrEP is an antiretroviral medication that can be taken by HIV-negative people to reduce the risk of HIV acquisition.
The project aimed to explore the barriers and facilitators to access PrEP among the following underserved audiences:
- Black African women;
- Trans and Non-binary people; and,
- Sex Workers.
Additionally, the project aimed to identify recommendations to increase PrEP uptake among specified underserved audiences.
The Approach
The project began with stakeholder interviews conducted with professionals from organisations that provided support or services to one or more of the three target audiences. Experts from the following organisations were interviewed:
- Basis Yorkshire;
- BHA for Equality;
- The Eddystone Trust;
- Dr Luke Wookey Indigo Gender Service; and,
- Prepster.
The interviews explored barriers and facilitators for underserved audiences to access PrEP, but also influenced the project methodology and overall recommendations.
Next, we collaborated with the following community and grass roots organisations to conduct qualitative research on Hitch’s behalf.
- Mojatu;
- BHA for Equality;
- The Eddystone Trust;
- Yorkshire MESMAC;
- Vista/Harbour Church; and,
- Portsmouth City of Sanctuary.
Additionally, we collaborated with three individuals who identified as Trans or Non-binary, with experience delivering workshops and conducting research, to reach Trans or Non-binary individuals.
Hitch provided training, support, and resources to enable organisations to conduct focus groups or 20-minute in-depth interviews.
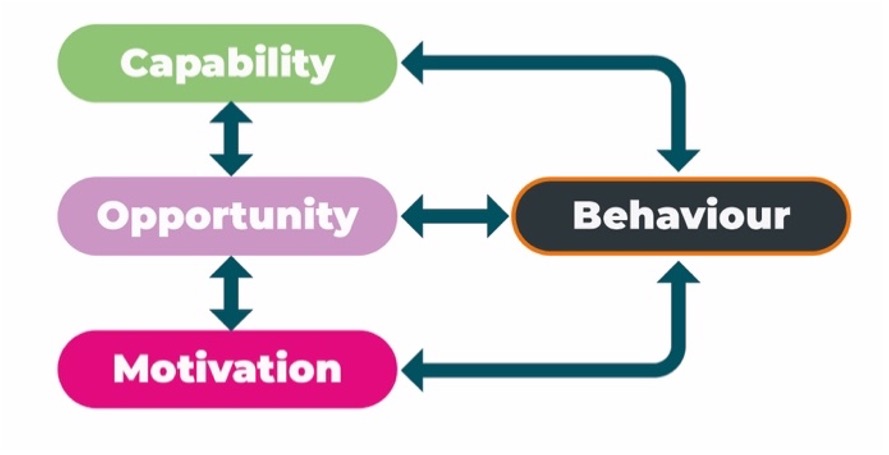
Discussion guides and resources were developed using the COM-B model for behaviour change as a framework for questions. The model states that a behaviour occurs as a result of three interacting factors: Capability (psychological and physical capability), Opportunity (physical and social) and Motivation (reflective and automatic).
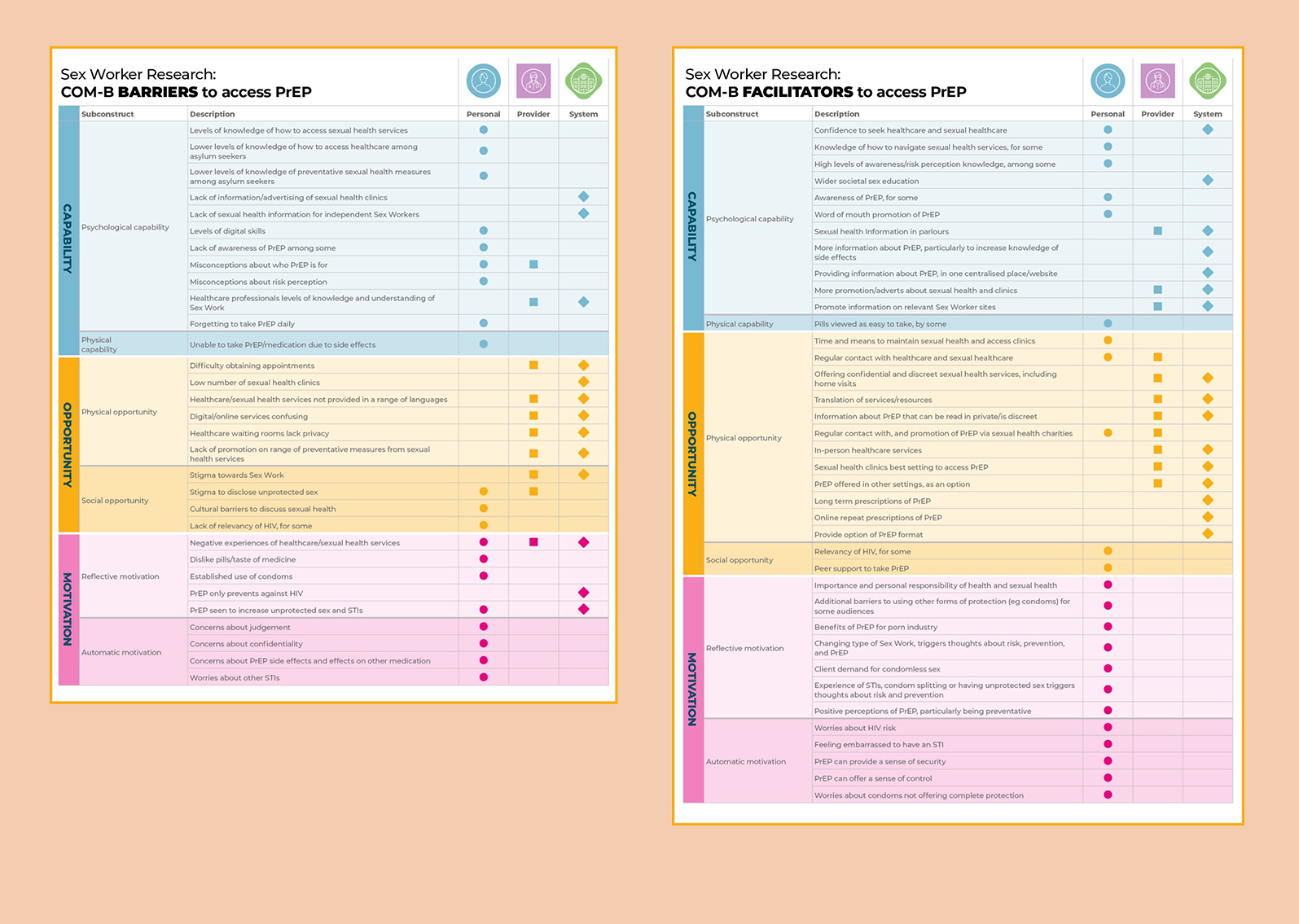
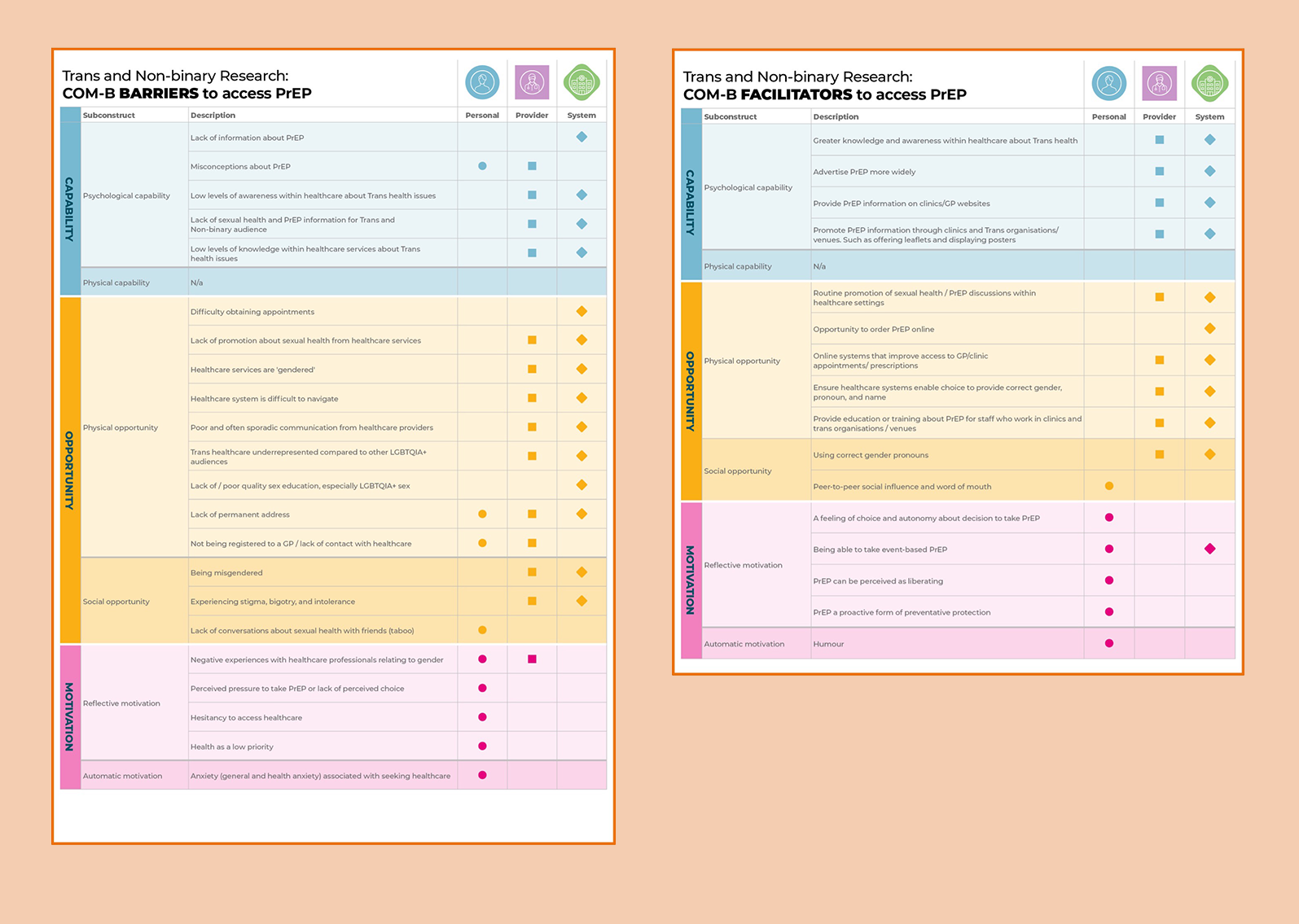
Data was collected and analysed. Thematic Content Analysis was used to identify themes which were coded as a barrier or facilitator and labelled as relevant for Personal (individual), community, society), Provider(primary or secondary healthcare, commissioner behaviour), or System (wider political or economic factors).
This aimed to highlight the interlinked barriers and facilitators which impact access to PrEP, and to show that change at a provider and system level, will also be necessary to effect positive change. Key findings can be viewed in the summary tables below.
The Results
Key themes and recommendations from our analysis included:
- Psychological capability: as a starting point, awareness, and knowledge around the existence as well as what PrEP is for was sometimes limited amongst the audiences as well as providers. Awareness raising at personal and provider level was therefore a key step to influence on increasing its uptake.
- Physical opportunity: at a system level, improved access to healthcare and sexual health services to increase PrEP uptake was mentioned across all audiences including access, format, variety of settings and approach to appointments and support.
- Social opportunity: stigma, whether it be societal, or prejudice within healthcare and sexual healthcare settings was also a key barrier across audiences, despite social opportunity factors generally being mentioned less. Tackling stigma at not only personal but provider as well as system level seems essential.
- Automatic motivation: Worries and concerns were present among all audiences around the potential side effects, efficacy of PrEP, and adherence to taking a daily pill for example. Again, this reinforced the point that increasing confidence and knowledge around PrEP at a system and provider level would be key.
- Reflective motivation: Previous experiences of accessing healthcare and sexual health services as well as how highly sexual health was prioritised amongst participants, were identified as both a facilitator or barrier to PrEP uptake across all audiences. We found that those experiences and prioritisation were very diverse across and amongst the groups.
Recommendations
A workshop was held to explore the key findings from the research and to use the Behaviour Change Wheel to identify recommendations.
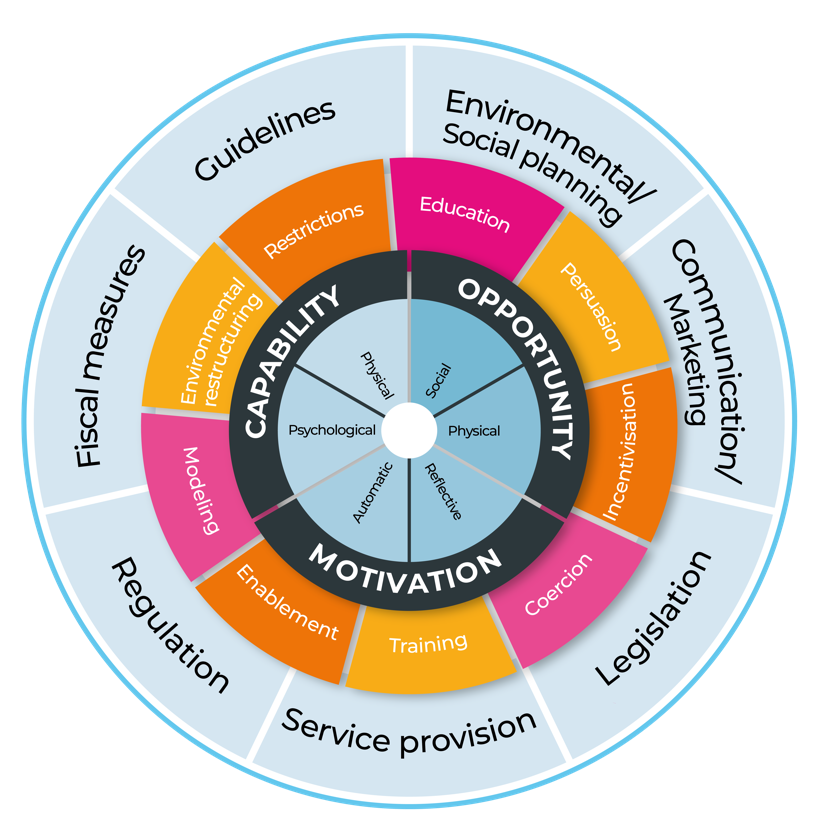
Recommendations were identified and again coded as relevant for a personal, provider or system level. Suggested recommendations included the creation of a peer-educator network, moving away from a criteria-based model to assess PrEP candidacy and providing sexual health support in non-clinic settings.
You can read the full report here.
If you would like to find out more about this or any other behavioural insights projects, please get in touch.